I’ve been meaning to write a blog about the new weight loss drugs for months now, but every time I start, I find myself having trouble with what I want to say, especially since so many of the anti-diet and fat-positive activists I admire have already written such important and insightful pieces on these drugs. For anyone looking for some in-depth research study analysis, I want to point you towards Ragen Chastain, a speaker, writer, and amazing fat activist, in addition to being a certified “statistics nerd” (her words, not mine!). Her Weight and Healthcare Substack is an invaluable resource that takes a hard look at “weight science, weight stigma and what evidence, ethics, and lived experience teach us about best healthcare practices and public health for higher weight people.” Ragen is adept at sifting through the research studies that the drug companies publish to sell the efficacy of these drugs and finding the myriad issues, conflicts of interest, and straight-up bad statistics that these studies exhibit. So please read what she has written on the topic of GLP-1 agonists.
In this piece, I am not going to get into the science behind how GLP-1 agonists such as Ozempic and Wegovy actually work. Instead, I want to talk about how these drugs (and the weight loss drugs that came before them) have become such a lightning rod in the discussion of weight. I was a teenager in the 90s, and I clearly remember when the drug Fenfluramine/Phentermine (Fen-Phen) entered the weight loss scene. There was such a fervor about it on the nightly news, and the marketing by the drug companies was intense. It was touted as a “miracle drug” that could “cure” o*esity, and everyone was going to their doctor to get a prescription. I also remember the news stories that came out. Famously, there was one in the Boston Herald about how Fen-Phen was linked to mitral valve dysfunction, pulmonary hypertension, and other cardiac abnormalities. Subsequently, it was removed from the market due to these risks. It took years before people were convinced that the harms that these medications caused outweighed the “benefits” of weight loss for higher weight people.
There has been a seemingly significant theoretical shift in the medical community over the past few years regarding higher weight (the “o” words”) and weight loss. Unlike previous decades, when people were told that their high weight was their “fault” and was caused by their “unhealthy lifestyle behaviors,” many medical professionals are now putting forth the message that one’s weight is largely out of one’s control (true) and is not necessarily due to “unhealthy lifestyle behaviors” (also true). Most physicians acknowledge that the BMI is a flawed measurement and that there are many factors that play into health other than weight (true again). But instead of pivoting away from using weight as an indicator of health, there has been a push by the medical community to classify o*esity and o*erweight as “chronic health conditions” that must be managed over one’s lifetime. In essence, the medical community is saying that while being fat isn’t your “fault,” it is still a problem and one that needs to be managed.
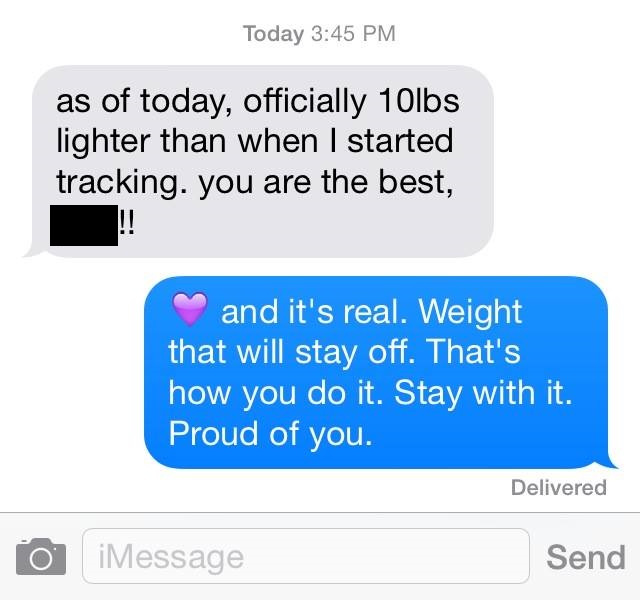
In our fat-phobic, image-obsessed culture, it makes sense why these new “miracle weight loss drugs” are creating such a stir. Higher weight people are being told, “Hey, we know that your weight is out of your control, but we can help you manage your ‘condition’ with these medications!” In addition, there is a lot of pressure on higher weight people to “get healthy” (even if many of them are healthy by every measure other than weight), and losing weight is still seen as something that will improve people’s health. The marketing that the drug companies have put forth is simply astounding. I feel like I can’t watch a TV show, peruse social media, or even read the New York Times without sponsored content popping up about these drugs. Add to this all of the celebrities and influencers who have been publicizing their weight loss “success,” I would be surprised if any person in a larger body wouldn’t be affected. Currently, I am in a small-mid fat, abled body, and I’d be lying if I said that I hadn’t thought about turning to these drugs. I can only imagine how those who are in much larger bodies than mine and/or in disabled bodies are tempted to try them.
The studies that have been put forth by Novo Nordisk (the drug company who makes Wegovy and Ozempic) have shown that while participants lost about two pounds per month over a 68-week time period (during which they were also dieting and exercising 30 minutes per day, six days per week), at 60 weeks, those who were still taking the medication experienced a plateau in their weight loss, and in a follow-up study the following year, two thirds of the weight they had lost was regained. Conveniently, the studies all concluded at the second year of testing, as we know that the majority of weight regain occurs between two to five years post weight loss attempt. Novo Nordisk also reported that taking their medication leads to positive health outcomes, but a closer look at their studies shows that there were no statistically significant improvements in HBA1C (a measure of diabetes), triglycerides, cholesterol, or inflammation markers.
I don’t blame anyone who feels like they need to try these drugs. For some folks, losing 10-15% of their body weight (the average weight loss reported by researchers) could feel like it makes a huge difference in their quality of life. What I find distressing about these drugs is how hard they are being pushed by the media and medical community despite the long list of side effects and potentially harmful health outcomes that can occur. Wegovy has a Boxed Warning (the FDA’s most serious warning) due to it increasing one’s risk for thyroid cancer, acute pancreatitis, acute gallbladder disease, stomach paralysis, as well as an increase in suicidal ideation, among other risks. But it seems that the medical community feels that losing weight is worth the risk to fat people’s lives. That even though folks report nausea, diarrhea, vomiting, constipation, and stomach pain while on these drugs, it’s okay as it is just the price to pay for one to become “healthy.”
I wish that instead of telling higher weight people that their weight is a problem that can be “solved” by taking these medications, the medical community could instead focus its energy on reducing weight stigma in healthcare, as this (along with weight cycling or yo-yo dieting and healthcare inequalities) has been found to have much more of a profoundly negative effect than weight on one’s health. I wish that we lived in a society that didn’t prize thinness so much. And I wish that everyone could see that weight is just another human characteristic that exists on a continuum and that bodily diversity is a real thing, not something that has to be “managed” or “controlled.”