Many of our colleagues shared articles, blog posts, and memes on social media to commemorate the day. One particular meme caught my attention because it read in part, “Families are not to blame, and can be the patients’ and providers’ best allies in treatment.”
To be candid, that statement is only partially true. On one hand, eating disorders can certainly arise in the midst of even the most loving and supportive family dynamics. On the other hand, environment is an important factor in the development of eating disorders, and this broad term that encompasses television, social media, print media, teachers, friends, coaches, co-workers, and many other influences also includes family.
Neither Joanne nor myself is here to pass judgment on anybody. Parenting is hard work, and all of us, parents and otherwise, make mistakes sometimes despite our best intentions. If we are to help families become the supportive allies that the meme correctly states they can be, then we must acknowledge the reality that even well-meaning and loving parents sometimes inadvertently contribute to the problem.
This month, Joanne and I discuss some of the most common mistakes parents make that can promote or exacerbate an eating disorder or otherwise hinder their child’s nutrition care, and we suggest alternative behaviors that can be more helpful. Joanne tackles the behaviors most related to eating disorders while I address others that I see in my side of the practice, although overlap certainly exists between the two.
Mistake 1: Modeling disordered behavior
“I can’t do moderation,” one of my patients insisted. She was 12 years old. With both of her parents out of the room, she explained to me how her parents oscillate between restriction and overconsumption. The former might take the shape of cleanses, clearing the house of “junk food,” enrolling in weight-loss programs, or other similar actions, while the latter might manifest itself through binges, lamenting their eating behaviors, or expressing concerns about a food “addiction” or feeling out of control.
The patient in question was well aware when one of her parents was about to transition from one state to another. “You cracked the seal!” her mother reportedly exclaims to her father (or vice versa) when a “bad” food is brought into the house. Because this is the behavior modeled in my patient’s household, no wonder she similarly feels, at such a young age, already destined for and incapable of anything beyond an all-or-nothing relationship with food as well.
Improvement: Model a healthy relationship with food
Children often learn through observation. Family meals in particular are an excellent time for parents to model their healthy relationship with food. Serve and consume a wide variety of foods. Destroy the good/bad food dichotomy by incorporating “bad” foods and showing that one is neither guilty for having them nor virtuous for sticking solely to “good” foods.
Similarly, keep a wide variety of foods in the house, as attempts to restrict the food supply typically backfire sooner or later. Children are bound to encounter “bad” food at friends’ houses, camp, and other environments, so better to help them build a healthy relationship with these foods early in life before they grow into young adults who do not know how to handle the newfound freedom that accompanies all-you-can-eat college dining halls.
In order to model a healthy relationship with food, parents must first of all have one. Be candid with yourself and realize that the best way to help your child might be to recognize and seek help and support for your own eating issues.
Mistake 2: Putting too much responsibility on the child
Encouraging autonomy and empowering children have their upsides, but parents sometimes take these actions too far. They step so far back that children are left without the parental support that they need to succeed. Parents might leave their children alone with us for more time than would be ideal, decline invitations to meet with us without the children or to check in with us between sessions, opt not to reinforce at home the ideas we discuss in session, or fail to implement action steps that necessitate parental involvement.
Improvement: Work together as a team
Just as children of all ages look to their parents for a variety of resources, everything from physical needs to unconditional love, they need similar help with their nutrition. Children have their own feeding responsibilities, but so do parents. In order to suss out who is responsible for what, parents must actively participate in the process. Initially, parents may not see eye to eye with us or have questions or concerns about our approach, and these thoughts are best expressed in private so as not to confuse the child with conflicting paradigms. In short, working together as a team tends to yield the most fruitful results.
Mistake 3: Assuming their children can lose weight because they did it themselves
Many of the children at our practice have parents who are high achievers. Through hard work, discipline, sacrifice, and other life choices and factors, they have reached the pinnacle of their respective fields. Some of these parents have applied these same traits to their own weight-loss endeavors with similar results. They assume that if their children take a similar path, they will reach the same outcome.
Improvement: Differentiate between typical and atypical results
If you have lost weight and kept it off, recognize that you are the exception, not the rule. Approximately 95% of people who attempt to lose weight will regain it one to five years down the road, and roughly 60% of these individuals will end up heavier than they were at baseline. Weight regain is common even if someone maintains the behaviors that promoted the weight loss in the first place.
Contrary to popular myth, our weight is largely out of our hands. The calories-in-versus-calories-out paradigm is a gross oversimplification of the complexities affecting weight regulation. While we might be able to manipulate our body size through behavior changes for a short while, biological mechanisms promoting weight regain almost always win out in the end.
Even genetics and behaviors together do not tell the whole story. For every Griffey or Boone family, we have hundreds of major league ballplayers whose offspring will never make it in the pros. Set aside the notion that what worked for parents will work for a child, and accept that your child may never lose weight and keep it off no matter what he or she does.
Mistake 4: Encouraging weight loss
A desire to lose weight leads to dieting, which is a predictor for eating disorders, worse health, and ultimate weight gain. Parents may understand the dangers and futility of dieting and instead encourage “lifestyle change.” Unbeknownst to them, the behaviors they have in mind, such as restricting calories or certain food groups, keeping a food journal, weighing or measuring portions, or staving off hunger by filling up on liquids or low-calorie foods, are still tricks of the dieting trade. Different packaging, but same contents.
Improvement: Promote size acceptance
Weight stigma is real and widespread. Children encounter it on the playground, on television, on social media, in the classroom, and maybe even at the pediatrician’s office, but they do not have to face it at home. Promote size acceptance and discuss the stigma they inevitably bump into as they move about the world. An additional and important lesson: Teach them not to contribute to said stigma.
Mistake 5: Talking about “health” as a euphemism for “weight”
Sometimes parents have a sense of the dangers associated with focusing on a child’s weight, so they substitute in the word “health” instead. Children are perceptive, however, and they learn about our cultural obsession with weight and size at an early age. When their parents say, “I just want you to be healthy,” they interpret this in context and hear, “I just want you to lose weight.” When they start talking to the big kid in the family about “health” and bring him to a dietitian while his skinnier siblings receive no such treatment, trust me, he knows exactly what is going on.
Improvement: Recognize that health and weight are not synonymous
Health and weight are not nearly as synonymous as we have been led to believe. Studies have shown that weight loss does not automatically lead to better health, and other research that controlled for behaviors found that health risks between groups of people of different body weights were nearly identical when engaging in similar behaviors. If health itself is indeed the priority, then apply it to everyone in the family, regardless of body size.
She Said
June 2nd was World Eating Disorders Action Day, during which numerous organizations and activists all over the world brought to light the prevalence of eating disorders (ED) and the need for comprehensive treatment. Jonah and I noticed a meme that was circulating on that day which outlined nine facts about EDs. While overall I felt like the meme was accurate and could be quite helpful for those unfamiliar with EDs, I felt like one of the “truths” was not completely accurate. This “truth” states, “Families are not to blame, and can be the patients’ and providers’ best allies in treatment.” My issue does not lie with the second part of the sentence, as I fully believe that parents can be wonderful allies in helping someone recover from an ED. But I do not agree with the statement that families are not to blame.
Let me be clear: I am not saying that it is solely the parents’ fault if their child develops an ED. But absolving parents of any blame doesn’t ring true to me. As in most diseases, genetics play a large role as does environment. One way of thinking about it is this saying: “Genetics load the gun, but environment pulls the trigger.” Well, parents are part of the child’s environment, and therefore they can contribute (even unwittingly) to the development of their child’s ED.
99% of the time, parents are acting out of love for their child. They don’t want their child to suffer and only hope that he or she will be happy and healthy. But even with the best intentions, sometimes parents (and other family members) can inadvertently trigger an ED in a genetically predisposed patient. The following are some examples of how this can occur:
Example #1: The parent speaks negatively about his or her own body.
This might be surprising to some people, but children of parents who speak disparagingly about their own bodies (i.e., not their child’s body) are more likely to develop issues with eating and body image. I’ve had numerous patients whose parents only tell the patient how beautiful/handsome/perfect he or she is, or that there is nothing wrong with the child’s body. However, oftentimes the child will overhear their parent complaining about their own “love handles,” saggy body parts, or “unsightly bulges,” and even though these comments aren’t directed at the child, he or she learns to internalize these messages and can start to believe that his or her body is “wrong” too. The best way to prevent this from happening is for parents to avoid negatively talking about their own bodies, especially in the presence of their child. All bodies are good bodies, and stressing this message can help kids develop a more positive body image.
Example #2: The parent puts too much responsibility on the child and does not take an active role in his or her ED recovery.
Sometimes I encounter parents who want to take a step back from their child’s ED, as they believe that the child should be in charge of his or her recovery. While I agree that the patient needs to take an active role, most kids are dependent on their parents for food, as parents are the ones who go grocery shopping and who do the meal prep and planning. A child who is dealing with an ED cannot be counted on to feed himself or herself appropriately. Very few kids with EDs take the initiative to prepare a snack or meal for themselves. I had one patient that often would skip meals and snacks because she knew that her parents weren’t watching her. My advice would be that parents need to take an active role in their child’s ED recovery, especially if that child is a younger teenager. This means that parents might need to supervise meals and snacks, make sure that there are ample and appropriate food choices in the house, and hold the child accountable for food eaten outside of the house. Regarding the latter, signs may suggest that a child is not following her meal plan while at school, for example. In such instances, parents have the responsibility to arrange for a teacher or school nurse to supervise the child’s eating to ensure compliance with the meal plan.
Example #3: The parent encourages their child to lose weight.
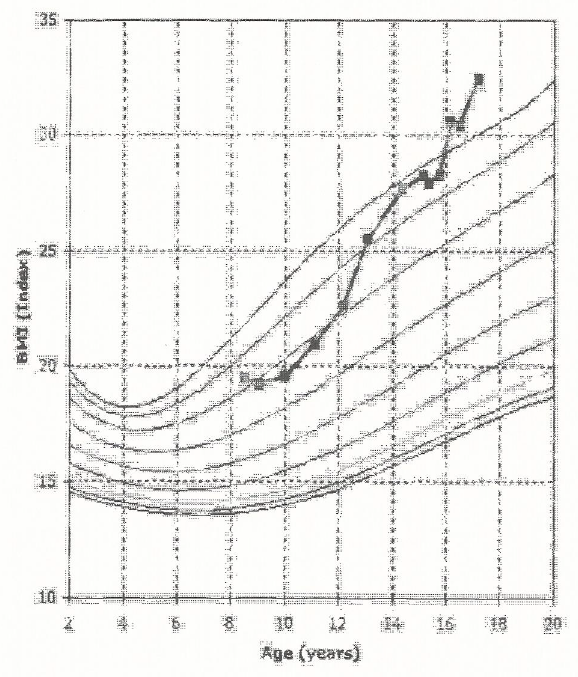
This is a tough one. In our fatphobic and fearmongering culture, being overweight or obese is seen as a terrible fate. With the help of Michelle Obama, every parent is vigilant about their child becoming a part of the “childhood obesity epidemic.” Even if a parent feels like their child is “fine,” pediatricians can scare parents into seeing their child’s weight as a ticking time bomb. I’ve had too many patients to count whose parents bring them in because their doctor wants the child to lose weight. In some cases, these kids are encouraged to go on diets, and they receive praise for every pound lost. I had one patient in particular whose parents promised her a new iPad if she lost a certain amount of weight. Obviously, I feel that encouraging one’s child to lose weight is very problematic. Study after study has shown that kids who start dieting from an early age are actually more likely to become overweight or obese in adulthood. In other words, the end result is the exact opposite of what these parents are hoping for. My best advice is to stop focusing on your child’s weight. Instead, focus on his or her health, as we know that health and weight are not necessarily synonymous. Also, I would recommend talking with the child’s pediatrician (without the child present) to discuss taking the focus off the child’s weight, as negative messages about the child’s weight can lead to a preoccupation with food and even development of an ED.
Thus, while I really agree overall with the “truths” outlined by the meme, I would modify #2 to say that family dynamics can play a role in the development of an ED. While it is true that parents are not solely to blame for their child developing an ED, they can use some of the above strategies to make it less likely that their child will go down that treacherous path.