Wow, I am hard pressed to remember an instance when something I read made me as angry as Juliann Schaeffer’s article in Today’s Dietitian entitled “Dietitians and Their Weight Struggles.”
In summary, the article contains quotes from dietitians who offer their opinions as to whether or not a dietitian’s weight and appearance should matter. Although the piece improves at the end when some sanity and rationality is injected into it, the beginning quotes from one of my fellow dietitians are so shamefully off base that I feel deeply embarrassed to be associated with her.
“If someone has a weight issue, then in my opinion, they should choose a specialty that does not conflict with being overweight.”
“If you can’t make it work for you, how can you make the case for someone else?”
“. . . the reality is that health care is a business, and people do judge you by appearance. Is it right or wrong? That doesn’t make a difference. It’s a business, and it is what it is whether we like it or not.”
“I wouldn’t think much of advice from a cardiologist if I knew he had had a heart attack.”
So wait, are we dietitians supposed to list our BMIs on our resumes and websites now, or how does this work?
It is one thing for some personal trainers, chiropractors, life coaches, “nutritionists,” therapists, doctors, and other dietitian wannabes to go outside the scope of their expertise and give harmful dietary guidance, but when an actual dietitian represents the profession the way she has there is just no excuse for it. This is our wheelhouse. We should be better than that.
When I was an intern, I had a rotation in a bariatric surgery clinic where two dietitians worked. One was heavier, one was leaner. Some patients did not want to work with the heavier one because they questioned, “Look how heavy she is; how can she possibly help me?” Yet other patients did not want to work with the leaner dietitian because they worried, “Look how skinny she is; how can she possibly relate to what it is like to be fat?”
Last year, a new patient told me she almost cancelled her appointment because she was intimidated by what a “great athlete” I was. Just a few months ago, another new patient came to me all impressed that I had “beaten cancer.” Well, no, I did no such thing. She had misunderstood my online autobiography. When I told her that, she deflated like a balloon.
Let’s get real for a moment. The whole notion that a practitioner has to look or behave a certain way in order to help patients is incorrect. Out of all the questions I asked the surgeons I met with before my most recent back surgery, I never thought to ask who among them has back problems. But I should have because if a surgeon has back problems then it is logical to conclude he or she cannot help me with my issues, right? Or wait, I want a surgeon with back problems because he or she can relate to my experience, is that how it goes?
How about just finding the surgeon whose approach, experience, and demeanor made me feel most comfortable and confident? I know, crazy me and my outlandish notions.
During my first year as a personal trainer, few members were interested in my services. Although I had good relationships with many of them and they routinely asked me questions about exercise, few were willing to cross the line of actually hiring me. However, after I took two months off to ride my bike across the country, suddenly members were booking sessions with me left and right and my boss began to refer new clients my way, too. Other trainers treated me and my opinions with more respect. The gym even gave me a raise without me asking for it.
Come on.
Sure, more money and clients were great, but the driving force behind the upturn in business was so ridiculous that I felt insulted. It took riding my bicycle 4,000 miles, up and down mountain ranges, through all sorts of weather, for my expertise to be recognized and taken seriously? The ride did not make me a better trainer. If anything, I was a worse trainer after my trip because I was rusty from not having worked in two months. But hey, perception is all that matters to some people.
Right now, I have a patient who wants to be a CrossFit coach and feels she needs to lose 15-25 pounds in order to be taken seriously by potential clients. Sure, she has room for changes in her lifestyle, just like we all do, but she generally eats well and takes great care of herself. As disappointing as it is for her to hear, it seems her body just naturally belongs 15-25 pounds heavier than she would like it to be. Do I push her further down the path she feels obligated to follow, risking perhaps disordered eating or an eating disorder, as she sacrifices health for a number and a look, or do I guide her towards the reality that she can be a great trainer no matter her weight and appearance?
Due to my surgery, it has been seven weeks since I lifted weights and did any physical activity in earnest. Muscle atrophy is setting in. My shoulders and chest are smaller. My six pack is gone.
Am I a worse dietitian now than I was two months ago?
What if you did not know that major surgery had affected my fitness and you came in here and saw a scrawny dietitian without any context? Would you have less confidence in me than if you knew about my operation?
What if I had not undergone surgery and I just decided to take two months off from working out?
What if I had a healthy relationship with both physical activity and food, but my body just happened to be thinner, less muscular, or heavier than society feels its dietitians should look? Would you go elsewhere?
I have blogged about my athletic accomplishments, such as my mountain running, on a small handful of occasions because it can enhance patient care for them to understand that I am a human being with a life outside of this office and I face challenges just like everybody else. Perhaps patients garner some inspiration from those postings, but if anybody reads one and then comes to see me with the mindset, “Jonah is thin and Jonah is an athlete; therefore, he can help me,” God, that would just make me want to take all of the posts down. I just cannot be part of that act.
The purpose of self-disclosure is to enhance patient care, not to serve as an advertisement, not to capitalize on misconstrued ideas, and certainly not for a practitioner to defend or justify his or her behaviors or body shape.
I disagree with the notion that health care is a business. The first priority should be patient care, not money. If the dietitian I quoted earlier had her priorities in order, she would be helping to reeducate her patients and change a culture of misunderstanding rather than playing into it for profit. Giving people what they want and expect for the sake of financial reward does not justify providing poor care and perpetuating a myth.
Or maybe I should just play along and take up steroids, lest patients go elsewhere because I no longer look the part, right?
Come on.
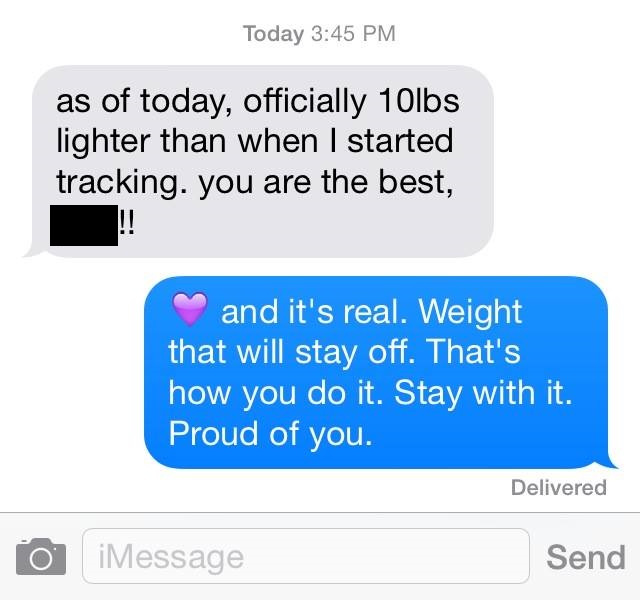 The above text exchange appeared in my Facebook feed, placed there by a personal trainer (whose name I blacked out from the image) who shared it to promote his business, a testimony to his prowess and the results he can bring to his clients who are seeking to lose weight.
The above text exchange appeared in my Facebook feed, placed there by a personal trainer (whose name I blacked out from the image) who shared it to promote his business, a testimony to his prowess and the results he can bring to his clients who are seeking to lose weight.