He Said
Halloween is when I first learned the meaning of the word “nauseous.” After returning home from trick or treating, I sat at the kitchen table eating candy until I no longer felt well. “Do you feel nauseous?” my mom asked. A loose definition formed in my childhood mind: Nauseous (adjective): Feeling completely gross from eating too much Halloween candy.
My brother, in contrast, always paced himself. While I blew through my own candy in a few days tops, he made his candy last for weeks, if not months. Eventually I realized that eating small amounts of candy at a time not only spared me from feeling nauseous, but the candy lasted longer. Preservation became fun, and at some point I started freezing candy. As springtime flowers bloomed, I would be eating last fall’s frozen Snickers.
Upon returning home from trick or treating, my brother and I dumped out our candy sacks, sorted our bounties into piles by kinds of candies, and traded with each other so we each had our favorites. In order to make our trades with each other, we each needed a foundational hierarchy of our candy likes and dislikes so we each knew which pieces we wished to keep and obtain more of and which ones we hoped to trade. In other words, we had to mindfully eat our candy in order to assess enjoyment.
Halloween and its associated candy provide opportunities for children to build their relationships with food. The healthiest relationships are built on a foundation of internal-cue recognitions and responses: having the ability to not only ask ourselves questions like “Am I hungry?” “How hungry am I?” and “What is it that I really want?” but more importantly, to be in touch with our bodies enough to be able to appropriately answer.
Building these skills involves trial and error. As I did on that Halloween so long ago, sometimes kids overeat and regret it. Sometimes they burn through their stash too quickly, not even truly enjoying a large portion of it, and wish they had conserved some for later. It is through these and similar lessons that we build the intuitive-eating skills that can serve us so well throughout our lives.
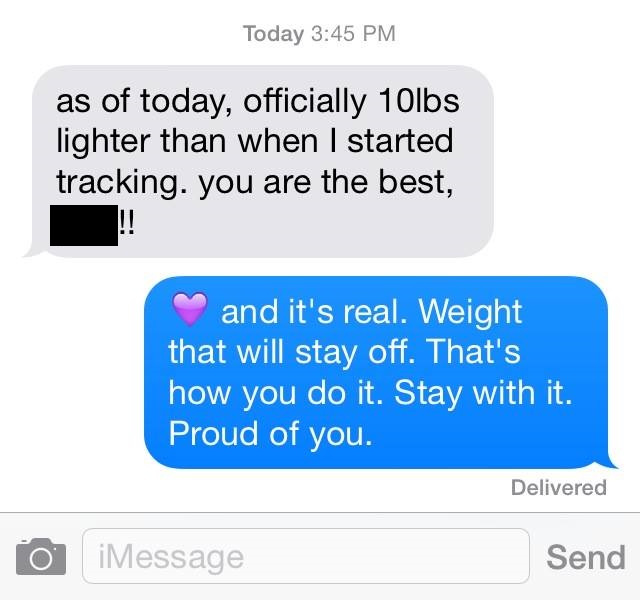
The alternative is to regulate children’s candy experience for them by forcing or coercing them to donate, trade, or throw out all or some of their candy, or by rationing the candy for them. Using external cues to regulate our eating may seem to work in the short term, but in the long run the approach almost always fails us. One particular patient comes to mind, a teenage girl who ignores her body’s hunger signals and eats according to the commands of an app. She tells me that she does not trust herself to listen to her body and that obeying the app is already “ingrained” in her. I think of the countless adults who sit across the table from me, fold their arms, lean back, and say, “Just tell me what to eat,” because for most of their lives they have been taught that they cannot trust themselves.
Well-intentioned parents want to help, but the assistance is often misplaced. Help your children to build their relationships with food by giving them the freedom to manage their Halloween candy themselves. Consider prompting your children to ask themselves how hungry they are and what do they really want before the eating begins, but not in a leading or coercive way. Give them the space to answer honestly and to follow up their candy experiences with more candid questions: “How full am I?” “How am I feeling now?” “How did I enjoy it?” and “What, if anything, would I do differently next time I have candy?” Give them the freedom to make mistakes and learn through experience, for it is partly through these lessons that we build healthy relationships with food.
She Said
The other day, Jonah told me about a local news story he had seen about a bunch of people who are now going to put signs on their front doors proclaiming that they are a “candy-free” house and that, as such, they will not be handing out any candy on Halloween this year. Instead, these individuals will be handing out small toys to the youngsters who come trick-or-treating to their door. Of course, the intention of these individuals is to not promote the “obesity epidemic” by handing out sugary treats to little ones.
The first thing that came to my mind about Halloween candy and kids was, “What would Ellyn Satter say?” Ellyn is a registered dietitian and eating specialist focusing primarily on children. She has written a number of pivotal books about how to feed children and how to prevent and/or help rectify problematic eating early on to promote a healthy relationship with food in years to come.
As luck would have it, Ellyn wrote an article in 2008 about the topic of Halloween candy and kids. In her opinion, she believes that Halloween candy should be treated the same way other sweets are treated and that the child needs to learn how to manage his sweets and how to “keep sweets in proportion to the other food he eats.” She cites a 2003 research study that found that girls that were “treat-deprived” (i.e., were restricted by their mothers in particular around treats and sweets) were more likely to overeat forbidden foods even if they weren’t hungry. Conversely, the study found that girls that were allowed treats on a regular basis ate them moderately and sometimes not at all.
Given the above study, Ellyn’s advice is to use Halloween candy as a “learning opportunity,” in which the child should work toward being able to manage his or her candy stash with minimal interference by the parent. What does that look like? Well, she would suggest that upon returning from trick-or-treating, the parent should let the child “lay out his booty” of Halloween candy, sort it out, and “eat as much of it as he wants.” After letting the child do this on the evening of Halloween and the next day, the child should put away the rest of the candy, and it will then be “relegated to meal- and snack-time: a couple of small pieces at meals for dessert and as much as he wants for snack time.” She goes on to say that “if [the child] can follow the rules, he gets to keep control of the stash. Otherwise [the parent does], on the assumption that as soon as the child can manage it, he gets to keep it.” Finally, she recommends offering milk with the candy to make sure the child is getting some good nutrition.
Now, when I first read the above, I found my inner skeptic coming up front and center. How could one possibly trust that his or her child could regulate his or her sweets intake? Isn’t that the parent’s job? Otherwise, wouldn’t we have a bunch of little kids gorging themselves on any sweets they could get their hands on? What’s next? Letting kids start drinking at a young age to help them learn to do so moderately as adults? It all sounded a bit too much to me.
But the more I thought about it, the more it made sense. By taking the taboo off sweets and treats, kids will be less likely to overdo it when they are faced with them. I have a colleague who regularly has a rotation of sweet treats and salty snacks in her house and does not limit her kids around this. What ends up happening, she says, is that her kids don’t see these foods as “off-limits” and therefore not so tempting. They know that if they want these foods, they can have them, but since they are always available, the forbiddenness is no longer an issue, and they eat them in moderation or sometimes not at all.
So what’s the take-home message from the above? Restricting sweets and treats can lead kids (and adults) to view these foods as “forbidden” and then when faced with them, they will find themselves overdoing it on these foods even if they aren’t hungry or in the mood for them. By incorporating these types of foods into one’s meals and snacks on a regular basis, they become less charged, and the individual will view them simply as part of their diet, not as forbidden fruit.